Background
 Figure 1. (Click to enlarge) |
 Figure 2. (Click to enlarge) |
A 41-year-old cognitively impaired man who lives in a home for the mentally impaired is presented to the emergency department (ED) by his caregivers. His caregivers at the home noticed that, after washing the patient, 1 of 2 shaving blades present in the morning was missing. Although they hadn't witnessed it, they suspected that the patient had ingested the missing shaving blade. The caregivers, however, haven't noticed anything abnormal with the patient; he does not have any shortness of breath, stridor, wheezing, hemoptysis, vomiting, or upper gastrointestinal (GI) bleeding. At no point have the caregivers noticed the patient coughing or choking; however, they are still worried about the possibility that he might have ingested or aspirated the blade.
At baseline, the patient has unintelligible speech and, therefore, cannot be directly interviewed. The patient has been living in a residence for the mentally impaired for the past 31 years, and he is dependent on his caregivers for all of the activities of daily living. Apart from his mental underdevelopment, the patient suffers from epilepsy and has been previously investigated for Raynaud's disease; in addition, the patient's history is significant for an ejection systolic murmur. The murmur was first detected by echocardiography, which revealed normal left ventricular function and a slightly thickened mitral valve, with minimal regurgitation. He takes multiple medications, including dipyridamole 100 mg TID, phenytoin 100 mg TID, doxepin 25 mg BID, nitrazepam 5 mg nocte, carbamazepine 20 mg BID, nifedipine 10 mg BID, nortriptyline 25 mg TID, and risperidone 1 mg nocte.
On physical examination, the patient is not in any distress. His oral temperature is 98.6°F (37.0°C). His pulse is regular at 82 bpm and his blood pressure is 140/90 mm Hg. His oxygen saturation is 99% while breathing room air. A visual inspection of the oropharynx does not reveal the presence of a foreign body, and there is no evidence of any recent trauma, bleeding, or swelling. There is normal range of motion in the neck, and no evidence of stridor or respiratory difficulty is noted. On chest auscultation, there is good air entry bilaterally, and normal vesicular breathing is heard. His heart sounds reveal a 2/6 ejection systolic murmur. His abdomen is soft and nontender. Additionally, no distention or rebound is noted on the abdominal examination.
Laboratory investigations, including a complete blood cell (CBC) count, biochemistry, and coagulation screen, are ordered. The patient's white blood cell (WBC) count is 10.7 × 103/µL (10.7 × 109/L; normal range, 3.5-11× 103/µL), hemoglobin is 14.9 g/dL (149 g/L; normal range, 13-18g/dL), and platelets are 433 × 103/µL (433 × 109/L; normal range, 140-400 × 103/µL ). His serum chloride is 104.0 mEq/L (104.0 mmol/L; normal range, 98-106 mEq/L), creatinine is 0.94 mg/dL (83 µmol/L; normal range, 0.6-1.2 mg/dL), potassium is 4.4 mEq/L (4.4 mmol/L; normal range, 3.5-5.0 mEq/L), sodium is 143.0 mEq/L (143.0 mmol/L; 135-145 mEq/L), blood urea nitrogen is 23 mg/dL (8.2 mmol/L; normal range, 7-18 mg/dL), and blood glucose is 92 mg/dL (5.1 mmol/L; normal range, 70 - 110 mg/dL). The patient's coagulation profile is normal.
A chest radiograph (see Figure 1) and a supine abdominal radiograph are obtained (a lateral chest radiograph is not taken). The blade is not initially seen on the chest radiograph because it was camouflaged by its surroundings in the body; however, on further examination, the object is determined to be in a specific anatomic structure (see Figure 2 for a close-up view), the right main bronchus.
Discussion
 Figure 3. (Click to enlarge) |
 Figure 4. (Click to enlarge) |
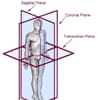 Figure 5. (Click to enlarge) |
|
The blade was not initially seen on the chest radiograph, but after further examination, the object was determined to be in the region of the right main bronchus. An ear, nose, and throat (ENT) consultation was obtained, and the patient was taken to the operating room, where a rigid bronchoscopy was performed. The bronchoscopy, however, failed to show anything in both bronchi and their main divisions. An esophagoscopy was subsequently performed, which showed that the shaving blade was actually in the middle third of the esophagus. The shaving blade was easily removed via esophagoscopy.
Although the anteroposterior chest radiograph seemed to show that the blade was in the right main bronchus in a sagittal orientation, the patient was in no respiratory distress. The abdominal radiograph revealed that the patient had severe scoliosis; therefore, the chest radiograph was a bit rotated, which resulted in the shaving blade appearing to be in the coronal plane on the anteroposterior chest radiograph. This finding indicated that the blade was in the esophagus. A lateral chest radiograph would have helped illustrate this as well. As a result of the initial suspicion of a razor blade in the airway, however, it was deemed safer to take the patient immediately to the operating room than delay treatment initiation.[5]
An ingested foreign body is a common emergency case. In 1999, the American Association of Poison Control documented 182,105 incidents of foreign body ingestion by patients younger than 20 years of age; however, accurate figures are difficult to obtain because many cases go unnoticed or are not reported. It is estimated that around 1,500 deaths related to foreign body ingestion occur annually in the United States.[2]
Patients of any age can be affected. The most common groups involved are children 1-5 years of age, adult patients with psychiatric problems or intellectual impairment, and prisoners (including "drug mules", who are people that transport drugs by hiding them within their bodies). Children less than 1 year of age may present with foreign body ingestion as well, although this is usually through the involvement of a sibling.[1,2,3]
There are several common sites where ingested foreign bodies can become impacted. In the esophagus, foreign bodies usually become impacted at the level of the cricopharyngeus (C-6), at the level of the aortic arch (T-4), and at the lower esophageal sphincter (T-11). Beyond the esophagus, foreign body impactions usually occur at the pylorus of the stomach, the C-bend of the duodenum, and at the ileocecal valve. In the colon, impactions typically occur at the hepatic and splenic flexures.[3]
The narrowest part of the esophagus is the cricopharyngeus (also known as the upper esophageal sphincter), which is the lowest part of the throat. Anything which has passed through the cricopharyngeus will most likely pass through the rest of the GI tract without any problems. In fact, 90% of ingested foreign bodies will spontaneously pass. Less than 1% of foreign body ingestions result in serious morbidity.[2,4]
The types of objects swallowed vary tremendously, including fish and poultry bones, coins, blades, toys, dentures, etc. The signs and symptoms of foreign body ingestion vary as well. These include blood in the saliva; coughing; drooling; dysphagia; odynophagia; fever; food refusal; the sensation of a foreign body in the throat; gagging; irritability; pain in the neck, throat, or chest; recurrent aspiration pneumonia; respiratory distress; stridor; tachypnea or dyspnea; vomiting; and wheezing.[4,5]
A small foreign body in the throat, such as a fish bone, will usually only scratch the pharyngeal mucosa before passing down into the stomach; however, larger objects may impact in the hypopharynx or esophagus, which can lead to perforation, stricture formation, mediastinitis, tracheoesophageal fistula, or even perforation of the aorta. Impactions further down the GI tract can cause intestinal obstruction manifested by vomiting, abdominal pain, and distention, and can eventually lead to peritonitis.[4]
Management of a swallowed foreign body depends on the symptoms of the patient and on the location of the object. A careful history should be taken; in particular, the time of ingestion and the nature of the foreign body should be noted, as well as the likelihood of the object to be radiolucent or radiopaque. The principles of airway, breathing, and circulation (the "ABCs") should be observed. If there is any suspicion of airway obstruction, immediate action should be taken to protect the airway.[4]
If a foreign body is suspected to be in the throat, the clinician should carefully inspect the pharynx and larynx with the help of indirect laryngoscopy or, if tolerated, flexible nasopharyngoscopy. Particular attention should be paid to the tonsils and valleculae, where fishbones often become stuck. If the foreign body is suspected to be further down the GI tract, the clinician must determine whether it is in the esophagus or is distal to the esophagus. Posteroanterior and lateral chest radiographs should be taken together with a plain abdominal radiograph in order to establish the location of the object.[4]
Objects located in the esophagus should be removed. There are several methods for removing objects in the esophagus; these include endoscopy, Foley catheter extraction (by inflating the balloon distal to the object and pulling it up), and bougienage (objects are pushed into the stomach so that they can pass through the rest of the GI tract). Although all of these methods have been proven to be safe when performed by experienced operators, esophagoscopy is the one most commonly used. Some authors have indicated that blunt objects in the esophagus may be observed for 24 hours and removed if they have not progressed after that period. Button-style batteries or sharp objects in the esophagus should be removed immediately.[2,4]
The management of foreign objects located distal to the esophagus is dependant on whether the patient is symptomatic or not. If the patient is symptomatic (eg, signs of obstruction are present), prompt removal is required. If the patient is asymptomatic, various factors must be considered. Small blunt objects should be regularly followed using weekly radiographs (every 3 days for button-style batteries or for objects in the stomach). The parents of any children who have ingested foreign objects should be advised to monitor their child's stool for the ingested object. The object should be endoscopically or surgically removed if it has not passed through the pylorus within 3 days (48 hours for batteries), or if there is no progress within 1 week of the object having passed beyond the stomach.[2,4]
If the object is sharp (such as an open safety pin, bone, toothpick, needle, razor blade, or broken thermometer) and is located before the duodenal C-bend (or duodenal sweep), it should be endoscopically removed. If the sharp object is beyond the duodenal bend, daily radiographs should be obtained, and the object must be removed if it has not progressed after 3 days. Even safety pins and razor blades, however, usually pass without incident. Large objects (ie, ≥2-3 cm in children under 1 year of age, or ≥3-5 cm in older children) should also be treated with caution, as they may impact. Large objects should be removed if located before the duodenal bend. Large objects that are distal to the duodenal bend should be followed regularly and removed if they are not making any progress within 1 week.[2,3,4]
Button-style batteries merit special attention because of the potential for voltage burns and direct corrosive effects. These harmful effects may occur as early as 4 hours after ingestion. Batteries that are still in the stomach after 48 hours or that are >2 cm in diameter should be removed endoscopically; however, 85% of button batteries that progress beyond the duodenal sweep pass in less than 72 hours. The progress of the battery should be checked radiographically every 3-4 days.[2,3]
Clinicians should also suspect a chronically retained foreign body in the esophagus when patients present with persistent respiratory symptoms, such as cough, hoarseness, recurrent pneumonia, or stridor. Respiratory symptoms will predominate over time as paraesophageal tissue swelling compromises the adjacent trachea. Clinicians should also consider this diagnosis when a child is failing to thrive and/or refuses feeds.[4]
The patient in this case made a good postoperative recovery. He was discharged the following day after an overnight stay for observation.
Article exerpted from Medscape January 30, 2009


